Keratoconus
Corneal Crosslinking
Keratoconus is a progressive eye disease in which the cornea, which is usually round, begins to thin and bulge outwards into a cone shape. When this occurs, the misshapen cornea deflects light that is supposed to enter the retina, causing distorted vision. Keratoconus occurs in roughly 1 in 2000 people; however, it can occur in one or both eyes and symptoms often develop in adolescence or one’s early twenties, gradually progressing over time.
Causes of keratoconus
Keratoconus is caused by the gradual weakening and bulging of corneal tissue over time. This eye condition is believed to be caused by a combination of genetic and environmental factors and is also associated with excessive eye-rubbing, eye allergies and other connective tissue disorders where the tissues around the body are more elastic and stretchy than normal.
Symptoms
While many may only experience mild visual distortions in the early phases, as the condition progresses, symptoms of keratoconus may include:
- Worsening nearsightedness
- Distorted vision
- Blurry vision
- Eyestrain
- Sensitivity to light
- Frequent changes to a current eyeglass prescription
- Poor vision with glasses
Treatment of keratoconus
Keratoconus is often treated with new eyeglasses; however, if a new prescription doesn’t seem to help, rigid gas permeable or scleral contact lenses may be recommended. However, to maintain an acceptable level of vision, eventually, other treatments will be needed, especially if the shape of the cornea continues to deteriorate.
In these more advanced cases, a non-invasive treatment known as corneal collagen cross-linking (CXL) is highly effective at strengthening the cornea and preventing further bulging and vision loss. For some patients, a specialised laser procedure called PTK may be advised together with cross-linking to smooth the surface of the cornea so that contact lenses can be worn more comfortably.
In other cases, intrastromal ring segments may be implanted to modify the curvature of the cornea, and correct nearsightedness and astigmatism caused. Intacs which are clear, arc-shaped corneal inserts, can also be surgically implanted within the cornea to reshape the front surface of the eye, to enhance vision.
In more advanced cases of keratoconus and cases where the back layer of the cornea is also damaged, a corneal transplant may be the most effective treatment option. This involves the replacement of the damaged cornea with a healthy donor cornea. Dr York also performs a new partial thickness corneal transplant procedure for many Keratoconus patients. This procedure is called a Deep Anterior Lamellar Keratoplasty (DALK). In this procedure, only the front damaged part of the cornea is transplanted, and the healthy layer of your own cornea is left behind. This results in lower rejection rates, longer survival of the corneal graft, quicker recovery and increased strength of the bond between your own eye and the transplant (lower risk of traumatic graft rupture).
If you require a corneal transplant for advanced keratoconus, then Dr York will assess your eye and discuss the most suitable surgical option for you.
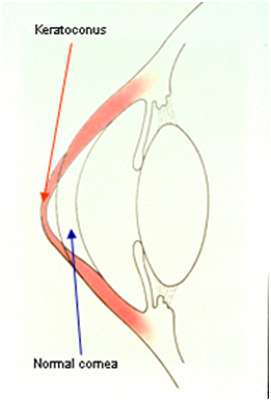 Diagram comparing keratoconus (red arrow) to an unaffected cornea (blue arrow)
Diagram comparing keratoconus (red arrow) to an unaffected cornea (blue arrow)
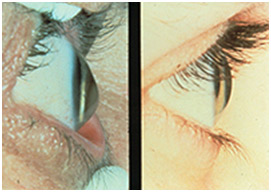 Advanced keratoconus (left) compared to an unaffected cornea (right)
Advanced keratoconus (left) compared to an unaffected cornea (right)
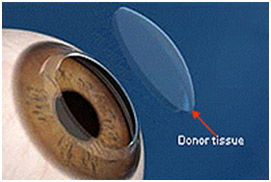 Tissue replaced in a corneal transplant
Tissue replaced in a corneal transplant


