Cornea Transplant Video
The cornea is the clear lens that covers the eye and is responsible for a large part of the eye’s focusing power. A number of conditions, including keratoconus, Fuchs’ dystrophy, scarring, swelling, thinning or clouding of the cornea due to infection or injury, can affect the cornea of the eye. Your corneas help bend and focus the light that enters your eyes so when misshapen or cloudy, a cornea transplant may be advised to restore proper vision and relieve pain.
What does a cornea transplant entail?
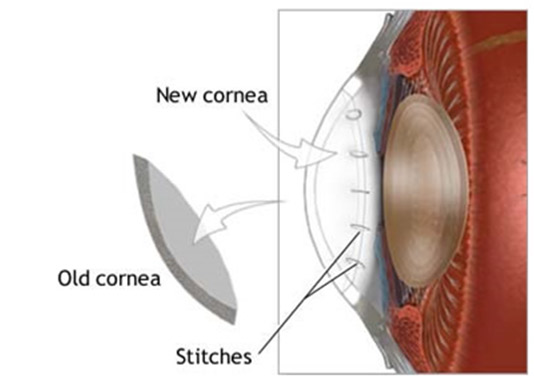
A cornea transplant involves the replacement of the scarred or damaged cornea with healthy donor tissue. It is usually advised for those who have difficulty with daily activities due to vision impairment and chronic eye pain. Depending on the damage to the cornea, a cornea transplant may be done to replace individual layers of the cornea, or to replace the entire cornea.
- Partial-thickness Corneal Transplant (Lamellar Keratoplasty)
When only individual layers are being replaced, it is known as partial-thickness corneal transplant and may be known as any of the following:- DSAEK (Descemet Stripping Automated Endothelial Keratoplasty)
- DMEK (Descemet Membrane Endothelial Keratoplasty)
- DALK (Deep Anterior Lamellar Keratoplasty)
This type of cornea transplant is indicated for those with Fuch’s dystrophy, keratoconus, corneal scarring, stromal corneal dystrophy, corneal failure after a cataract, glaucoma or retinal surgery, endothelial failure or rejection of a full transplant. Which layers are needed to be replaced will be determined by your ophthalmologist.
- Standard full thickness Corneal Transplant (Penetrating Keratoplasty)
When the entire cornea is being replaced, it is referred to as standard full-thickness corneal transplant and called a Penetrating Keratoplasty. This is generally advised for those patients with advanced keratoconus with severe scarring, severe herpetic scarring or a full-thickness traumatic injury.
How is a corneal transplant done?
Dr York can perform a corneal transplant using either local or general anaesthesia. For a full-thickness transplant, the damaged cornea is removed and replaced with a donor cornea. For a partial thickness transplant, only certain layers are removed and replaced. The transplant is then secured in place with tiny stitches.
What can be expected after the surgery?
You will need to arrange for someone to drive you after surgery. After a corneal transplant, you can expect some pain and discomfort for the next 2-3 weeks, and your vision will improve once the eye has healed, and the stitches have been removed. During recovery, you will be prescribed antibiotic and steroid eye drops as well as pain medication. You will be instructed to wear protective sunglasses and should be careful not to rub your eyes. You will be instructed to avoid any strenuous activity for at least one month of surgery.
Recovery will vary depending on the type of transplant and the way you heal; however, a partial-thickness transplant is generally less invasive, and thus recovery is quicker than with a full-thickness corneal transplant. It may take up to a year to fully recover from a full-thickness transplant (Penetrating Keratoplasty) or DALK transplant. For these patients, glasses or specially fitted contact lenses are often needed to obtain the best visual outcomes.
For those who have undergone a DMEK and DSAEK, visual improvement is much more rapid and usually occurs within 6 weeks of the date of surgery.